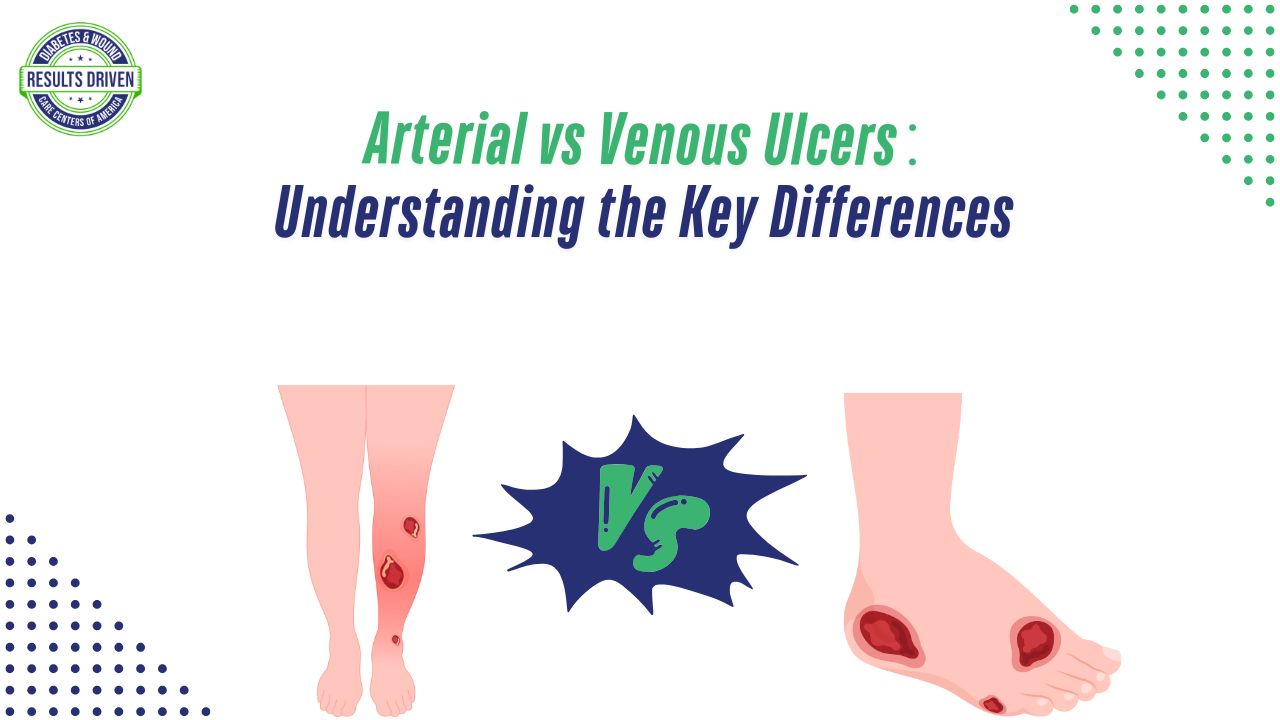
Arterial vs. Venous Ulcers: Understanding the Key Differences
What if a simple misdiagnosis could turn a manageable wound into a life-altering complication? Arterial and venous ulcers may appear similar at first glance, but they have distinct causes, symptoms, and treatment approaches. These ulcers significantly impact mobility, comfort, and overall quality of life, especially in older adults or those with chronic illnesses. Knowing the key differences is crucial for effective treatment and recovery. Let’s take a closer look at what sets arterial and venous ulcers apart and how they should be properly managed.
Arterial Ulcers: Causes, Symptoms, and Treatment
Arterial ulcers develop due to insufficient blood flow to the extremities. When arteries become narrowed or blocked, oxygen and essential nutrients fail to reach the tissues, leading to cell death and ulcer formation. This type of ulcer is most commonly associated with peripheral arterial disease (PAD), a condition caused by atherosclerosis, in which fatty deposits build up in the arteries and restrict circulation. Other contributing factors include smoking, diabetes, high cholesterol, and hypertension, all of which increase the risk of arterial blockages.
Symptoms of Arterial Ulcers
The location and appearance of arterial ulcers provide important clues for diagnosis. These ulcers typically form on the feet, toes, heels, or other pressure points, where blood supply is already limited. They have a dry, deep appearance, often with a well-defined, “punched-out” look. The wound base may appear black or necrotic due to tissue death. Unlike venous ulcers, arterial ulcers are extremely painful, with discomfort worsening when the leg is elevated and improving slightly when the limb is lowered.
Other warning signs of arterial ulcers include cold or pale skin on the affected limb, weak or absent pulses in the feet, and delayed capillary refill. In severe cases, gangrene may develop, increasing the risk of amputation if circulation is not restored.
Treatment of Arterial Ulcers
Managing arterial ulcers requires a multi-faceted approach focused on restoring blood flow, preventing infection, and supporting tissue healing. Revascularization procedures such as angioplasty, stent placement, or bypass surgery may be necessary to improve circulation. Proper wound care is also critical—this includes regular debridement to remove dead tissue, applying moisture-balanced dressings, and using topical or systemic antibiotics if infection is present.
Lifestyle modifications play a crucial role in preventing further complications. Quitting smoking, managing diabetes, controlling cholesterol levels, and maintaining healthy blood pressure can reduce the risk of additional arterial blockages. Patients with arterial ulcers should also avoid excessive pressure on their feet and wear specialized footwear to protect vulnerable areas.
Venous Ulcers: Causes, Symptoms, and Treatment
Venous ulcers occur due to chronic venous insufficiency (CVI), a condition in which the veins struggle to return blood to the heart. When venous valves weaken or become damaged, blood pools in the lower legs, leading to increased pressure in the veins. Over time, this high pressure damages the vein walls and surrounding tissues, resulting in fluid leakage, swelling, and skin breakdown.
Symptoms of Venous Ulcers
Venous ulcers typically develop on the lower legs, particularly near the ankles, in an area known as the gaiter region. Unlike arterial ulcers, which are deep and dry, venous ulcers are shallow with irregular, moist edges. The surrounding skin often appears discolored, swollen, or hardened due to chronic venous pressure. These ulcers may ooze fluid, making them prone to infection.
Pain levels in venous ulcers differ from arterial ulcers. Rather than severe, constant pain, venous ulcers tend to cause a dull, aching discomfort that worsens after prolonged standing and improves when the legs are elevated. Other associated symptoms include leg heaviness, itching, and varicose veins.
Treatment of Venous Ulcers
The primary goal in treating venous ulcers is to improve circulation and reduce swelling. Compression therapy, using compression stockings or bandages, is one of the most effective methods for promoting venous return and preventing fluid buildup in the legs. Elevating the legs above heart level for extended periods can also help reduce pressure and promote healing.
Wound care for venous ulcers involves keeping the wound moist with appropriate dressings, managing exudate, and performing regular debridement if needed. Advanced therapies such as sclerotherapy, laser vein ablation, or surgical interventions may be recommended to improve venous function and prevent ulcer recurrence.
Lifestyle changes such as maintaining a healthy weight, engaging in regular physical activity, and avoiding prolonged periods of standing or sitting can also aid in managing venous insufficiency. For patients with severe venous disease, vein procedures may help correct the underlying issue and reduce the risk of future ulcers.
Key Differences Between Arterial and Venous Ulcers
Arterial and venous ulcers may share some similarities, but their causes, symptoms, and treatments differ significantly. Misidentification can lead to ineffective treatment, delayed healing, or even severe complications.
Cause
Arterial ulcers result from poor arterial blood flow due to conditions like PAD or atherosclerosis, whereas venous ulcers stem from chronic venous insufficiency, which leads to high venous pressure and fluid leakage.
Location
Arterial ulcers primarily develop on the feet, toes, and pressure points, where circulation is most compromised. Venous ulcers, on the other hand, occur in the lower legs, particularly near the ankles.
Appearance
Arterial ulcers are deep, dry, and well-defined, often appearing black or necrotic. Venous ulcers are shallow, moist, and irregular, frequently accompanied by swollen or discolored skin.
Pain Levels
Arterial ulcers cause severe pain that worsens with leg elevation, while venous ulcers produce an aching sensation that improves when the legs are elevated.
Treatment Focus
Arterial ulcer treatment focuses on restoring circulation through procedures like angioplasty or bypass surgery, while venous ulcer treatment prioritizes improving venous return through compression therapy and leg elevation.
The Importance of Proper Diagnosis and Early Intervention
Because arterial and venous ulcers require different treatments, proper diagnosis is essential. Healthcare providers use diagnostic tools such as Doppler ultrasound, Ankle-Brachial Index (ABI) tests, and venous duplex scans to determine whether a patient has arterial or venous insufficiency. A correct diagnosis ensures that treatment is targeted and effective, reducing the risk of complications.
Delaying treatment or misidentifying the type of ulcer can lead to serious consequences, including chronic infections, severe pain, and even limb amputation in the case of advanced arterial disease. Seeking medical attention at the first sign of a non-healing wound can make a significant difference in the outcome.
Taking the Right Steps Toward Healing
Understanding the differences between arterial and venous ulcers is key to receiving the correct treatment and promoting faster healing. Whether restoring blood flow for arterial ulcers or managing venous pressure for venous ulcers, early intervention is critical. If you or a loved one is dealing with a slow-healing wound, consult a wound care specialist as soon as possible to develop an appropriate treatment plan.
By working with healthcare professionals, following recommended treatments, and making lifestyle adjustments, you can take control of your health and prevent these ulcers from worsening. When it comes to wound care, timely action can mean the difference between prolonged complications and a successful recovery.